The Client
The client is a leading global provider of technology-enabled risk, benefits and integrated business solutions, located across 65 countries.
The Challenges
- The information for bills & claims was not integrated into one platform. Users spent time running multiple reports to get detailed information on medical bills, claims and payments, various fee information and manually consolidated the data for detailed analysis.
- There was no access to near real-time data due to the existing legacy application. This led to a delay in decision-making.
- The application used by the client had limited visualization capabilities and was not flexible for self-service reporting.
The Objective
The client required a powerful analytical tool to unleash valuable insights from the embedded data in the Medical Bill review process. These insights would enable the end customers of the client to elevate their managed care and bill review process to a strategic and data-focused initiative that can drive ongoing program improvements in the organization. The tool needed to have flexible reporting capabilities, along with access to near real-time data.
The Solution
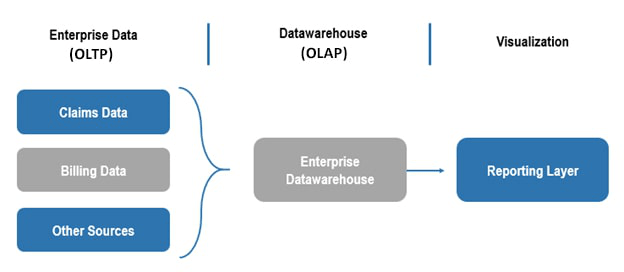
JK Tech as a solution partner analyzed the end-to-end process and designed a comprehensive bill-centric workflow by bringing the billing and claims data onto one platform. This enabled business users to analyze the key metrics of the bill review process and take the necessary actions to expedite the bill review process effectively. Key highlights of the solution are:
- Seamless integration of billing information with claims and payments data.
- Built Dashboards and reports with information on bill status, expenses, fees, payments to enable analysts and business users to derive key metrics in managed care.
- Tightly integrated the solution with data and user security, to ensure data confidentiality.
- Built scalable and reusable components to support ad-hoc reporting. Customized key functionalities of BO reporting, to accommodate the unique requirements of business users.
Solution Footprint – Comprehensive Care Analytics:
The Benefits
- A decrease in the average turn-around time of the billing process.
- Tracking metrics related to bill processing is much simpler and faster – approved, rejected and pending bills tracking, loss ratio, expense and claim reserve management.
- Analysis of key metrics for Telephone case management, Field case management, Pharmacy management, etc. through summarized dashboards and visualizations.
- Optimization of the utilization of physicians and provider networks.
- The solution helped reduce the usage and maintenance of multiple reporting systems.



